Abstract
Research Article
Management of acute tongue swelling
Siew Min Keh, Mohammad Hasan, Vamsidhar Vallamkondu and Muhammad Shakeel*
Published: 14 July, 2020 | Volume 4 - Issue 1 | Pages: 012-017
Background: Tongue swelling often presents as an acute upper airway obstruction.
Aim: To present a case series of patients presenting with an acute tongue swelling sharing our experience in managing these patients.
Subjects and methods: A retrospective analysis of consecutive patients presenting acutely to the emergency department (ED) at two institutions in Scotland. All patients were evaluated by an otolaryngologist for probable causes of tongue swelling. Data were collected on demographics, co-morbidities, clinical history, examination findings, acute airway management and subsequent care the patients needed.
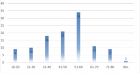
Results: A total of 32 patients (mean age ± STD, 61.6 ± 18.8; 65% male) were included in the study from two teaching hospitals. The most common presenting symptoms were difficulty in speaking (30/32, 94%) and dysphagia (27/32, 84%). Breathing difficulty was only observed in 8 of 32 patients (25%). Angiotensin converting enzyme (ACE) inhibitor’s induced angioedema was the most common cause (45%) for acute tongue swelling. Three (9.4%) patients required intubation; 2 (6.3%) on initial presentation. Two patients had emergency tracheostomy for breathing difficulties due to supraglottic swelling on flexible pharyngolaryngoscopy.
Conclusion: Acute tongue swelling is a life-threatening condition. The patients on ACE inhibitors would appear to be at higher risk of developing acute tongue swelling. Such patients with potentially compromised airway need to be treated in a facility where emergency intubation and tracheostomy can be performed at a short notice.
Read Full Article HTML DOI: 10.29328/journal.hor.1001020 Cite this Article Read Full Article PDF
Keywords:
Tongue swelling; Acute upper airway obstruction; Angioedema; Haematoma; Anaphylaxis; Allergy
References
- Moellman JJ, Bernstein JA, Lindsell C, Banerji A, Busse PJ, et al. A consensus parameter for the evaluation and management of angioedema in the emergency department. Acad Emerg Med. 2014; 21: 469-484. PubMed: https://pubmed.ncbi.nlm.nih.gov/24730413
- Banerji A, Clark S, Blanda M, LoVecchio F, Snyder B, et al. Multicenter study of patients with angiotensin-converting enzyme inhibitor-induced angioedema who present to the emergency department. Ann Allergy Asthma Immunol. 2008; 100: 327-332. PubMed: https://pubmed.ncbi.nlm.nih.gov/18450117/
- Bluestein HM, Hoover TA, Banerji AS, Camargo CA Jr, Reshef A,et al. Angiotensin-converting enzyme inhibitor-induced angioedema in a community hospital emergency department. Ann Allergy Asthma Immunol. 2009; 103: 502-507. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20084844
- Gabb GM, Ryan P, Wing LM, Hutchinson KA. Epidemiological study of angioedema and ACE inhibitors. Aust N Z J Med. 1996; 26: 777-782. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9028507
- Wood SM, Mann RD, Rawlins MD. Angio-oedema and urticaria associated with angiotensin converting enzyme inhibitors. Br Med J (Clin Res Ed). 1987; 294: 91-92. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1245098/
- Lunde H, Hedner T, Samuelsson O, Lötvall J, Andrén L, et al. Dyspnoea, asthma, and bronchospasm in relation to treatment with angiotensin converting enzyme inhibitors. BMJ. 1994; 308: 18-21. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2539116/
- Weiner JM. Failure to recognise the association of life-threatening angio-oedema and angiotensin-converting enzyme inhibitor therapy. Aust N Z J Med. 1995; 25: 241-242. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7487694
- Andrew N, Gabb G, Del Fante M. Aust Fam Physician. ACEI associated angioedema - a case study and review. 2011; 40: 985-988. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22146327
- Anderson MW, deShazo RD. Studies of the mechanism of angiotensin-converting enzyme (ACE) inhibitor-associated angioedema: the effect of an ACE inhibitor on cutaneous responses to bradykinin, codeine, and histamine. J Allergy Clin Immunol. 1990; 85: 856-858. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/2185292
- Ferner RE, Simpson JM, Rawlins MD. Effects of intradermal bradykinin after inhibition of angiotensin converting enzyme. Br Med J (Clin Res Ed). 1987; 294: 1119-1120. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/3034372
- Makani H, Messerli FH, Romero J, Wever-Pinzon O, Korniyenko A, et al. Meta-analysis of randomized trials of angioedema as an adverse event of renin-angiotensin system inhibitors. Am J Cardiol. 2012; 110: 383-391. PubMed: https://pubmed.ncbi.nlm.nih.gov/22521308/
- Mudd PA, Hooker EA, Stolz U, Hart KW, Bernstein JA, et al. Moellman. Emergency department evaluation of patients with angiotensin converting enzyme inhibitor associated angioedema. 2020; PubMed:
- Krogh Nielsen T, Bygum A, Rye Rasmussen E. Life-threatening angio-oedema after the first dose of an ACE inhibitor-not an anaphylactic reaction. BMJ Case Rep. 2016; 2016: bcr2016214364. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27229746
- Gilbert JD, Byard RW. Lethal manifestations of angioedema. Forensic Sci Med Pathol. 2019; 15; 494–497. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30390279
- Bozkurt S, Arslan ED, Köse A, Ayrık C, Yılmaz A, et al. Lingual angioedema after alteplase treatment in a patient with acute ischemic stroke. World J Emerg Med. 2015; 6: 74‐76. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4369536/
- Sezer Ö, Aydin AA, Bilge S, Arslan F, Arslan H. Acute dystonic reaction leading to lingual hematoma mimicking angioedema. Indian J Pharmacol. 2017; 49: 325‐327. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29326495
- Ishoo E, Shah UK, Grillone GA, Stram JR, Fuleihan NS. Predicting airway risk in angioedema: staging system based on presentation. Otolaryngol Head Neck Surg. 1999; 121: 263-268. PubMed: https://pubmed.ncbi.nlm.nih.gov/10471868/
- Al‐Khudari S, Loochtan MJ, Peterson E, Yaremchuk KL. Management of angiotensin‐converting enzyme inhibitor–induced angioedema. The Laryngoscope. 2011 121: 2327-2334. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4241279/
- Cicardi M, Aberer W, Banerji A, Bas M, et al. (European Academy of Allergy and Clinical Immunology). Classification, diagnosis, and approach to treatment for angioedema: consensus report from the Hereditary Angioedema International Working Group. Allergy. 2014; 69: 602-616. PubMed: https://pubmed.ncbi.nlm.nih.gov/24673465
- Maurer M, Magerl M, Ansotegui I, Aygören-Pürsün E, Betschel S, et al. The international WAO/EAACI guidelines for the management of hereditary angioedema – the 2017 revision and update. Allergy. 2018; 73: 73(8):1575-1596. PubMed: https://pubmed.ncbi.nlm.nih.gov/29318628/
- Cicardi M, Banerji A, Bracho F, Malbrán A, Rosenkranz B, et al. Icatibant, a new bradykinin-receptor antagonist, in hereditary angioedema. N Engl J Med. 2010; 363: 532-541. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4662377/
- Ostenfeld S, Bygum A, Rasmussen ER. Life-threatening ACE inhibitor-induced angio-oedema successfully treated with icatibant: a bradykinin receptor antagonist. BMJ Case Rep. 2015; 2015: bcr2015212891. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26498671
- Baş M, Greve J, Stelter K, et al. A randomized trial of icatibant in ACE-inhibitor-induced angioedema. N Engl J Med. 2015; 372: 418‐425. PubMed: https://pubmed.ncbi.nlm.nih.gov/25629740/
- Straka BT, Ramirez CE, Byrd JB, et al. Effect of bradykinin receptor antagonism on ACE inhibitor-associated angioedema. J Allergy Clin Immunol. 2017; 140: 242‐248.e2 PubMed: https://pubmed.ncbi.nlm.nih.gov/27913306
- Sinert R, Levy P, Bernstein JA, et al. Randomized Trial of Icatibant for Angiotensin-Converting Enzyme Inhibitor-Induced Upper Airway Angioedema. J Allergy Clin Immunol Pract. 2017; 5:1402‐1409.e3. PubMed: https://pubmed.ncbi.nlm.nih.gov/28552382/
Figures:
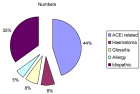
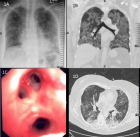
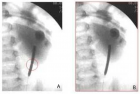
Figure 1

Figure 2
Similar Articles
-
Management of acute tongue swellingSiew Min Keh,Mohammad Hasan,Vamsidhar Vallamkondu,Muhammad Shakeel*. Management of acute tongue swelling. . 2020 doi: 10.29328/journal.hor.1001020; 4: 012-017
Recently Viewed
-
The Utility of Acupuncture in Sports Medicine: A Review of the Recent LiteratureMichael Malone*. The Utility of Acupuncture in Sports Medicine: A Review of the Recent Literature. J Sports Med Ther. 2017: doi: 10.29328/journal.jsmt.1001004; 2: 020-027
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Sex after Neurosurgery–Limitations, Recommendations, and the Impact on Patient’s Well-beingMor Levi Rivka*, Csaba L Dégi. Sex after Neurosurgery–Limitations, Recommendations, and the Impact on Patient’s Well-being. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001099; 8: 064-068
-
The effect of NLP-based approach to teaching surgical procedures to senior OBGYN residentsMitra Ahmad Soltani,Jamileh Jahanbakhsh*,Zahra Takhty,Azarmindokht Shojai,Hengameh Sheikh. The effect of NLP-based approach to teaching surgical procedures to senior OBGYN residents. Clin J Obstet Gynecol. 2021: doi: 10.29328/journal.cjog.1001075; 4: 001-002
-
Unilateral pleural effusion as the sole presentation of ovarian hyperstimulation syndrome (OHSS)Tarique Salman*,Suruchi Mohan,Yasmin Sana. Unilateral pleural effusion as the sole presentation of ovarian hyperstimulation syndrome (OHSS). Clin J Obstet Gynecol. 2020: doi: 10.29328/journal.cjog.1001074; 3: 182-184
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."