Case Report
Leiomyosarcoma of Maxillary Sinus – A Rare Clinical Entity

Sah BP1*, Chettri ST2, Karki S2, Shah SP1, Manandhar S1 and Jaiswal RK3
1Associate Professor, Department of Otorhinolaryngology and Head & Neck Surgery, B.P. Koirala Institute of Health Sciences, Dharan, Nepal2Professor, Department of Pathology, B.P. Koirala Institute of Health Sciences, Dharan, Nepal
3Senior Resident, Department of Otorhinolaryngology and Head & Neck Surgery, B.P. Koirala Institute of Health Sciences, Dharan, Nepal
*Address for Correspondence: Dr. Bajarang Prasad Sah, MS, Associate Professor, Department of Otorhinolaryngology and Head and neck Surgery, B.P. Koirala Institute of Health Sciences, Dharan, Nepal, Tel: +9779842030356; Email: [email protected]
Dates: Submitted: 25 June 2018; Approved: 16 July 2018; Published: 17 July 2018
How to cite this article: Sah BP, Chettri ST, Karki S, Shah SP, Manandhar S, et al. Leiomyosarcoma of Maxillary Sinus – A Rare Clinical Entity. Heighpubs Otolaryngol and Rhinol. 2018; 2: 001-005. DOI: 10.29328/journal.hor.1001015
Copyright License: © 2018 Sah BP, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Leiomyosarcoma is a malignant smooth-muscle tumor that has a predilection for the gastrointestinal and female genital tract and is a rare entity in the paranasal sinuses. It is locally fast-spreading and highly aggressive, and the prognosis is poor. We report a rare case of leiomyosarcoma of the maxilla in a patient who sought treatment for maxillary swelling, nasal obstruction with no epistaxis, orbital involvement or cervical lymph node metastasis. The patient underwent total maxillectomy followed by radiotherapy. At present after 5 years of follow up, he is symptom free with no recurrence.
Background
Leiomyosarcoma accounts for 6.5 % of all soft-tissue sarcomas, and only 3% of them arise in the head and neck [1]. Leiomyosarcoma of the head and neck are believed to be originated in the tunica media of the blood vessels or pluripotent mesenchymal cells. Leiomyosarcoma with regional lymph node involvement are also rare and cervical metastasis has been reported in 15% of leiomyosarcomas arising in the oral cavity [2]. Clinically, leiomyosarcoma is very aggressive and carries a poor prognosis. The 5-year survival rate with disease-free status is 23 % [3].
Leiomyosarcoma of nose and paranasal sinuses is very rare. When they occur in the sinonasal tract, the most common sites are the nasal cavity, the maxillary sinus, and the ethmoid sinus, in decreasing order. We report a rare case of leiomyosarcoma of the maxillary sinus.
Case Report
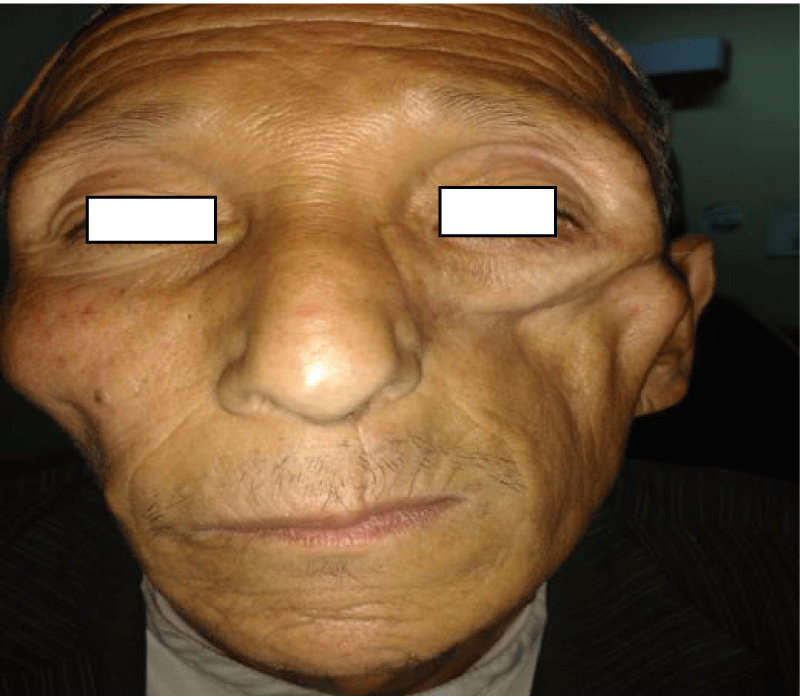
We report a 56-year male, farmer by occupation with a painless swelling on the left cheek region for 6 months. Since last 1 month he developed pain over the swelling associated with nasal obstruction. There was no epistaxis, proptosis and loose teeth. Clinical examination revealed a single globular swelling of 5 x 4 sq. cm present on the left side of face 4 cm lateral to midline, 2cm below the infraorbital rim and extending laterally to zygomatic process. Margins were well defined, firm to hard in consistency, non-tender, immobile, not adherent to skin but adherent to underlying structure, no impulse on cough and transillumination test was negative. There was adequate mouth opening with multiple nicotine staining of teeth. In the neck, bilaterally no palpable lymph nodes palpable (Figures 1,2).
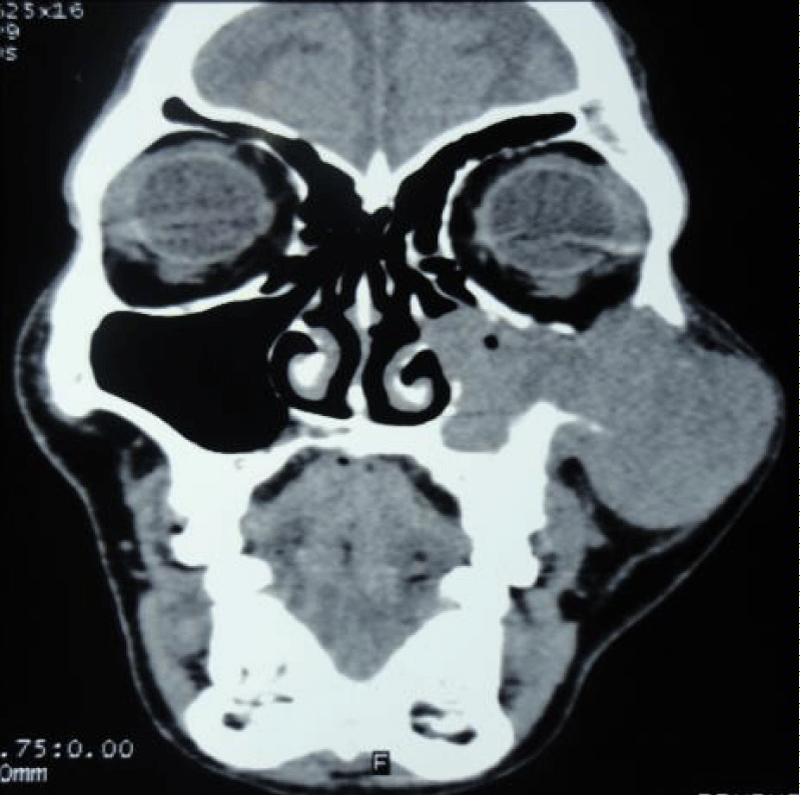
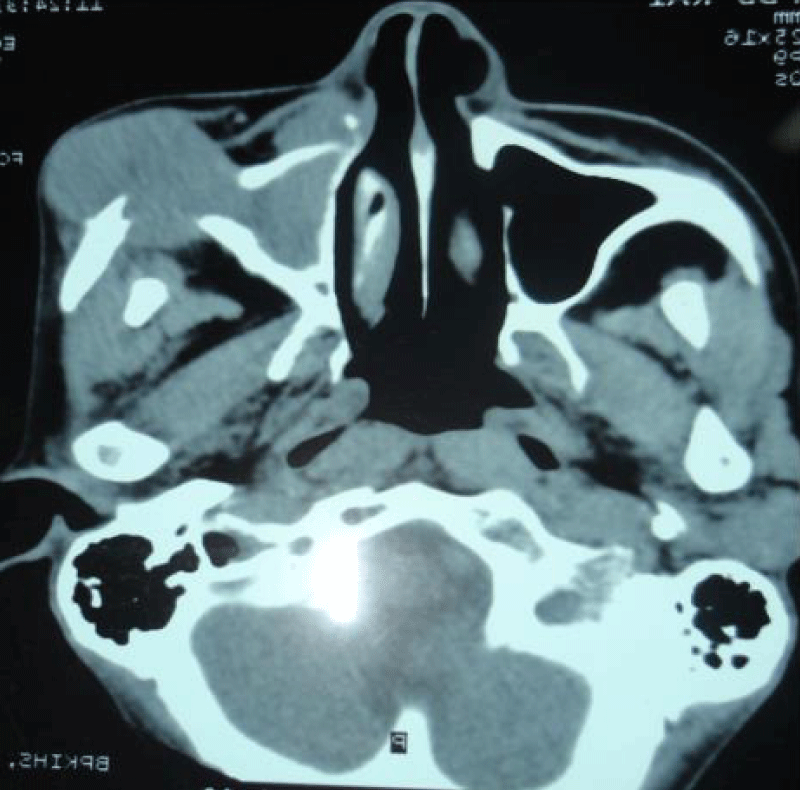
On Anterior Rhinoscopy, a fibrous band connecting the left inferior turbinate with the septum was present. No any bleeding sign, no any obvious nasal mass or bulging. All the cranial nerves were intact. A clinical diagnosis of the malignancy of left maxilla was made. Computed Tomography of Nose and Paranasal Sinuses revealed a soft tissue mass of 5 x 4 cm in the region of left zygomatic bone and left cheek. Laterally, it was causing destruction of part of zygomatic bone with focal bulge in the left cheek, maintaining the intervening fat plane with skin and subcutanous tissue. Medially, there was destruction of part of posterolateral and anterior wall of left maxillary sinus with extension into maxillary sinus and thinning of medial wall of left maxillary sinus with blockage of left ostemeatal complex and bulge into the left nasal cavity. Inferomedially, there was thinning and erosion of hard palate,alveolar process of maxilla on left side, left pterygoid plate, left medial and lateral pterygoid process. Superiorly, there was thinning and erosion of floor of left orbit with mass minimally bulging into left orbit. Inferiorly,there was extension to left infratemporal fossa with loss of intervening fat plane with temporalis and masseter muscle on the left side. The lesion was mildly heterogenously enhancing with few nonenchancing hypodense areas within. Soft tissue opacifications were seen in left maxillary sinus suggestive of retained secreations. The neck showed submental, bilateral submandibular and upper jugular lymph nodes, largest measuring 15mm (Figures 3,4).
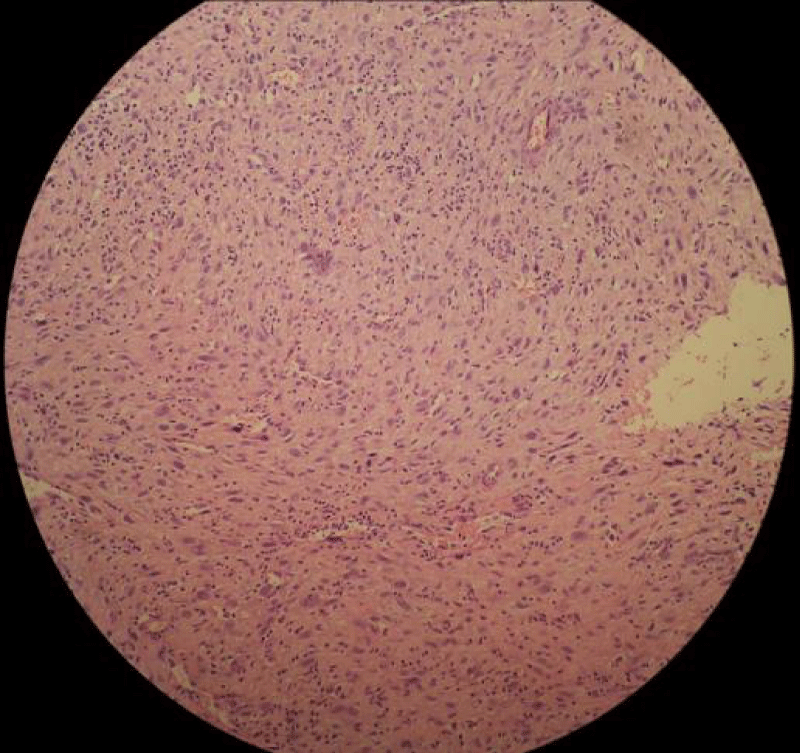
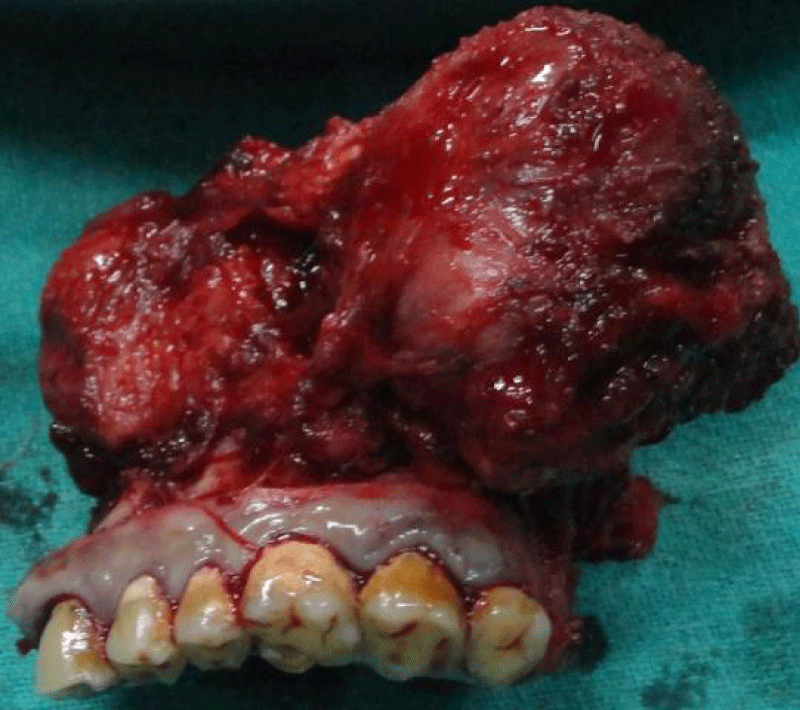
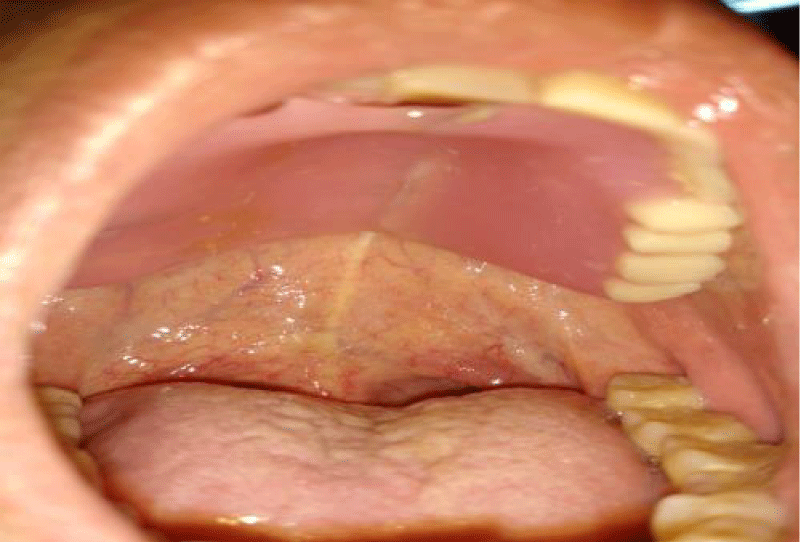
On Fine Needle Aspiration Cytology from the left maxillary region yielded blood mixed aspirate and the cells were arranged in large tissue fragments, sheets, cluster and singly.The individual spindle cells showed moderate pleomorphism with dense bipolar to fibrillary cytoplasam,bizare looking cells with irregular nuclear membrane and prominent nucleoli. The overall cytomorphological features were those of Malignant Mesenchymal Tumor (Figure 5). The patient underwent total maxillectomy by lateral rhinotomy approach. The surgical wound was closed primarily without any flap. An obturator plate was placed at the defect of the hard palate (Figure 6).
Analysis of the biopsy specimen revealed that the tumor tissue comprised of fascicles of spindle-shaped cells with eosinophilic cytoplasm and oval to elongated and blunt ended vesicular nuclei. Mitosis was conspicuous. Areas of necrosis, fibrosis, hyalinization, and inflammatory infiltrates were seen. The reticulin stain showed abundant reticulin fibers around individual tumor cells. The van Gieson’s and Masson’s trichrome stains showed smooth-muscle differentiation in the spindle cells. The tumour cells showed strong vimentin and smooth muscle actin (SMA) stains. These features were suggestive of leiomyosarcoma.
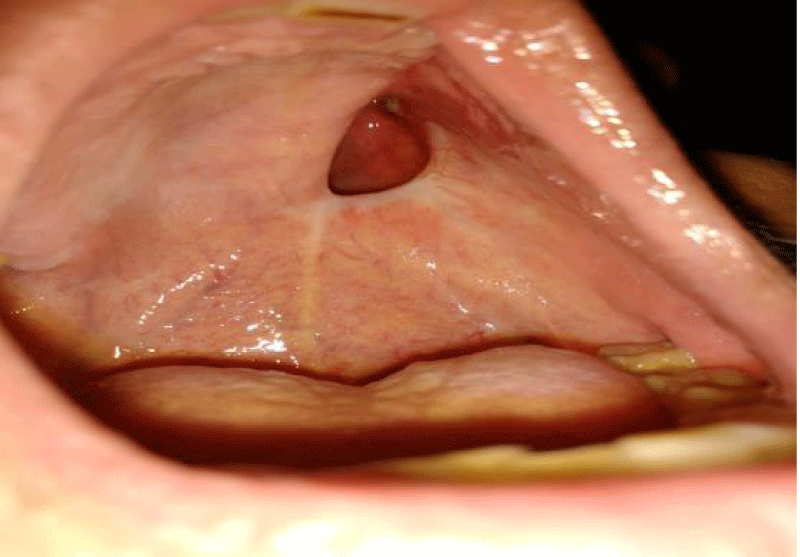
The patient received 33#/ 66Gy of radiotherapy. The patient is currently well and under regular follow up for the past 5 years. Clinical evaluation and nasal endoscopy on follow up revealed normal mucosa with no sign of locoregional recurrence as well as distant metastasis (Figures 7-10).
Discussion
Leiomyosarcoma are uncommon malignant neoplasams of smooth muscle origin that tend to occur in the alimentary tract, uterus and retroperitonuem. Leiomyosarcomas are very unusual soft tissue sarcomas of the head and neck region. The first case of leiomyosarcoma of nasal cavity and paranasal sinuses was reported in 1958 [4]. Since 1950, only 38 cases of leiomyosarcoma of the head and neck structures have been reported [5].
Leiomyosarcomas of the sinonasal tract are more common in men than in women. The average age of diagnosis is 50 years. Initial symptoms in order of decreasing frequency include nasal obstruction, epistaxis, facial pain, and facial swelling. Sinonasal tract leiomyosarcoma is characterized as locally aggressive with a low metastatic potential [1]. Our patient presented with painless facial swelling with nasal obstruction in the absence of epistaxis and locally invasive features. Sinonasal tract leiomyosarcoma is characterised as a locally aggressive lesion rather than having high metastatic potential [6]. The standard treatment is complete resection of the tumour with at least one cm margin. Radical resection alone having a high rate of local control but achieving a complete resection is usually not feasible due to anatomical constraints. Local recurrences are therefore common and a recurrence rate of 35-50% has been reported [7]. Metastasis occurs via hematogenous route most commonly to the lungs. Cervical metastasis, mostly due to contiguous spread has been reported in 15% cases [8].
In our case experience, the total maxillextomy with post operative radiotherapy is adequate and patient doing well without any local recurrences or distant metastatis in a follow up period of 5 years.
Conclusion
Leomyosarcoma of maxillary sinus is extremely rare. Accurate diagnosis, adequate surgical resection with adjuvent radiotherapy is the standard of care for such patient.
References
- Tanaka H, Westesson PL, Wilbur DC. Leiomyosarcoma of the maxillary sinus: CT and MRI findings. Br J Radiol. 1998; 71: 221-224. Ref.: https://tinyurl.com/y7sztea9
- Yamaguchi S, Nagasawa H, Suzuki T, Fujii E, Iwaki H, et al. Sarcomas of the oral and maxillofacial region : a review of 32 cases in 25 years. Clin Oral Invest. 2004; 8: 52-55. Ref.: https://tinyurl.com/y97npb62
- Schenberg ME, Slootweg PJ, Koole R. Leiomyosarcomas of the oral cavity. Report of four cases and review of the literature. J Craniomaxillofac Surg. 1993; 21: 342-347. Ref.: https://tinyurl.com/yclxrlfj
- Dropkin LR, Tang CK, Williams JR. Leiomyosarcoma of nasal cavity and paranasal sinuses. Ann Otol Rhinol Laryngol.1976; 85: 399-403. Ref.: https://tinyurl.com/ydayl3jg
- Dhingra S, Sethi A, Singh I, Sareen D. Leiomyosarcoma of the Maxillary Sinus: An Unusual Site of occurrence. Internet J Head Neck Surg. 2007; 2.
- Kuruvilla A, Weing BM, Humphrey DM, Heffner DK. Leiomyosarcoma of the sinonasal tract. Arch Otolarngol Head Neck Surg. 1990; 116: 1278-1286. Ref.: https://tinyurl.com/y9o5eeju
- Mindell RS, Calcaterra TC, Ward PH. Leiomyosarcoma of the head and neck. A review of the literature and report of 2 cases. Laryngoscope. 1975; 85: 904-910. Ref.: https://tinyurl.com/y9ye33qr
- Kazemian A, Kamian SH, Hosein MS, Azizi MR. Leiomyosarcoma of the tongue; Report of a case. Iran J Radiat Res. 2005; 3: 143-147.