More Information
Submitted: August 06, 2024 | Approved: August 22, 2024 | Published: August 23, 2024
How to cite this article: Redivo M, del Pilar Mingheira M, Long FF, Ruggeri CS. Laryngeal Xanthogranulomatosis: A Case Report. Heighpubs Otolaryngol Rhinol. 2024; 8(1): 001-003. Available from: https://dx.doi.org/10.29328/journal.hor.1001028.
DOI: 10.29328/journal.hor.1001028
Copyright License: © 2024 Redivo M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Xanthogranuloma; Histiocytes; Larynx; Transoral epiglottectomy
Laryngeal Xanthogranulomatosis: A Case Report
Micaela Redivo1, María del Pilar Mingheira1, Federica Fernandez Long1 and Carlos Santiago Ruggeri2*
1Residents, ENT Department, Hospital Italiano de Buenos Aires, Argentina
2Staff Physician, ENT Department, Hospital Italiano de Buenos Aires, Argentina
*Address for Correspondence: Carlos Santiago Ruggeri, Staff Physician, ENT Department, Hospital Italiano de Buenos Aires, Argentina, Email: [email protected]
Xanthogranulomatosis is an uncommon disease affecting non-Langerhans histiocytes.
Laryngeal involvement is very rare.
We describe the clinical case of an adult patient with disseminated xanthogranulomas affecting the supraglottic region of the larynx, leading to thickening and immobility of the epiglottis. The patient experienced inspiratory dyspnea on exertion. A transoral supraglottic epiglottectomy was performed, and a tracheostomy was subsequently required.
Xanthogranulomatosis is a rare disease of non-Langerhans histiocytes. Excessive proliferation of these cells can affect various organs and produce tumors. The juvenile form is the most common, while manifestations in adults are very rare. The pathogenesis of this disease is unknown and may be associated with malignant hematologic disorders. Laryngeal involvement can produce obstructive symptoms and may require surgical treatment.
We describe the clinical case of an adult patient with supraglottic xanthogranulomas that caused thickening and reduced mobility of the epiglottis, resulting in inspiratory dyspnea on exertion.
We performed a transoral suprahyoid epiglotectomy intending to improve inspiratory dyspnea.
The rarity of this pathology and its laryngeal location, together with the transoral surgical treatment that we performed, make the description of this clinical case of interest [1-3].
A 33-year-old male patient was referred by dermatology for bilateral nasal obstruction, dysphonia, and inspiratory dyspnea on exertion of 15 months duration. He had a family history of xanthogranulomatosis, with a biopsy from another center confirming xanthogranuloma. He also had facial and scrotal involvement.
He was treated with oral isotretinoin (20 mg/day) for 18 months, which halted disease progression, but symptoms recurred upon discontinuation of the medication. Inspection revealed multiple facial plaques affecting the eyelids. Anterior rhinoscopy showed greasy plaques (xanthomas) in the anterior nasal cavities. Video rhinoscopy and laryngoscopy revealed nasal lesions and isolated xanthomas on the posterior pharyngeal wall. The epiglottis and aryepiglottic folds were thickened by xanthomas. Vocal cord visualization was challenging, showing only the anterior part with normal characteristics; vocal cord mobility was preserved.
The epiglottis contacted the posterior pharyngeal wall and had limited mobility, obstructing glottic visualization.
Neck CT with contrast diagnosed thickening of the epiglottis and aryepiglottic folds. Chest CT showed bilateral subpleural para septal and centrilobular emphysema, peripheral interstitial thickening consistent with chronic bronchial disease, and bronchiectasis in the lower lung fields.
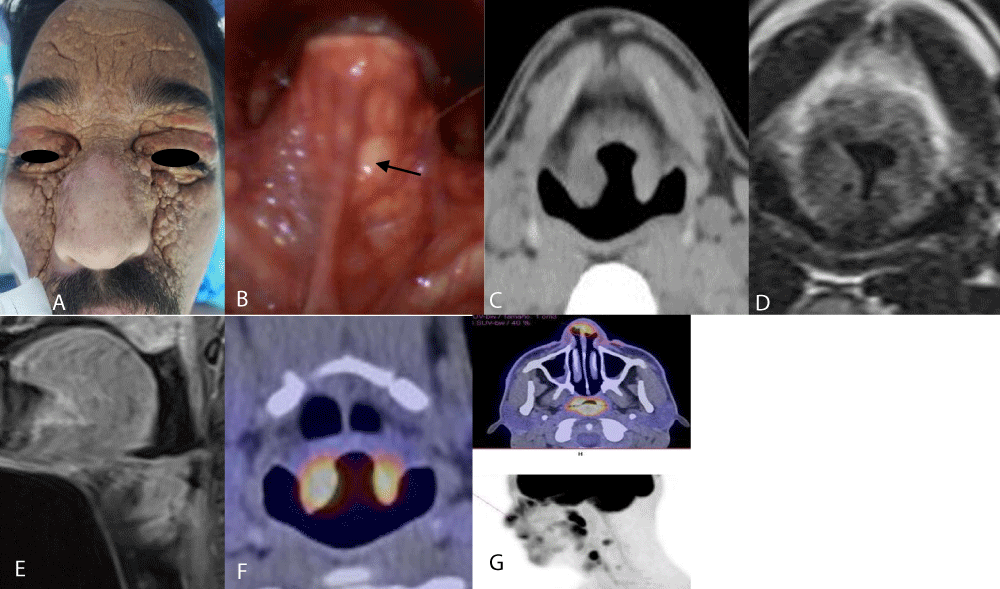
The neck MRI showed a thickening of the epiglottis and laryngeal crown, while the brain MRI was normal. PET-CT showed increased metabolism in facial thickening (SUVmax 8.3 in the nose) and bipalpebral area (SUVmax 8), as well as increased uptake in the aryepiglottic folds and bilateral scrotal area, ruling out distal visceral disease Figure 1.
Figure 1: Xanthogranulomatosis. A: Patient showing multiple facial and palpebral xanthomas. B: Thickened epiglottis due to xanthomas (black arrow indicates a xanthoma). C: Axial CT of the neck showing epiglottic thickening. D: Neck MRI showing thickening of the epiglottis and aryepiglottic folds. E: Sagittal MRI showing epiglottic thickening with reduced supraglottic space. F and G: PET-CT showing increased metabolism in the epiglottis and nasal vestibule.
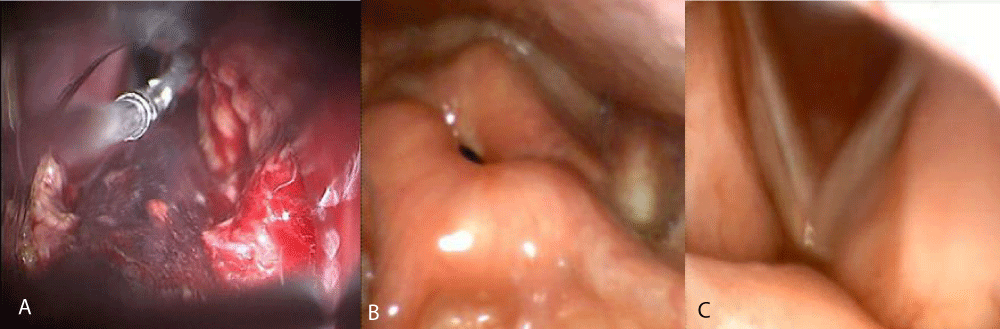
Due to progressive dyspnea, a partial transoral epiglottectomy with cautery was performed using a Bouchayez tip. Xanthomas from the aryepiglottic fold and left ventricular band were also resected Figure 2.
Figure 2: A: Partial supraglottic epiglottectomy and resection of xanthogranulomas in the aryepiglottic fold and ventricular band. B and C: Postoperative video-rhinoscopy showing residual epiglottis after supraglottic epiglottectomy and normal glottic space.
A functional swallowing study performed 24 hours after surgery showed aspiration only with liquids, leading to the initiation of an oral semi-solid diet and thickened liquids. The patient had a good recovery and was discharged 48 hours after surgery.
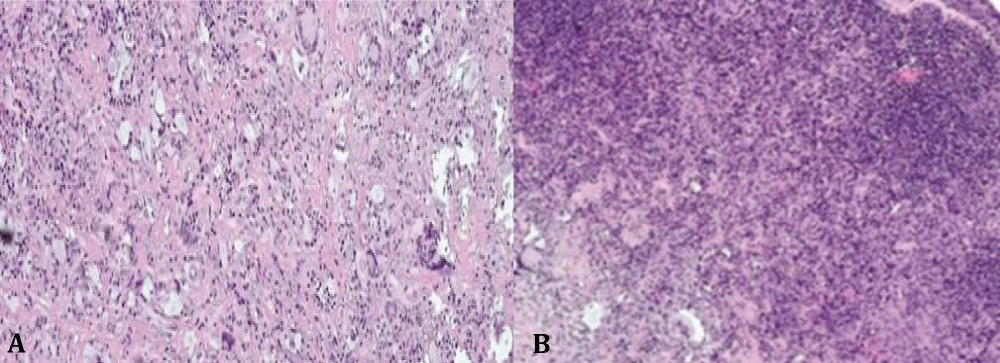
The histopathological study of the surgical specimen was reported as non-Langerhans histioid proliferation with xanthogranuloma-like areas Figure 3.
Figure 3: Supraglottic xanthogranuloma. A: Hematoxylin-eosin staining (200X) showing an infiltrate of histiocytes with clear, vacuolated cytoplasm and prominent nuclei associated with multinucleated giant cells. B: Hematoxylin-eosin staining (40X) showing respiratory epithelium with lympho-plasmocytic infiltration mixed with histiocytes.
Immunostaining was positive for CD68 and Factor XIIIa, and negative for S100 and CD1a. Molecular biology techniques did not detect mutations in codon 600 of the BRAF gene.
Swallowing rehabilitation was performed, and 30 days later, the patient could ingest liquids normally. Inspiratory dyspnea resolved. Three months later, the patient reported recurrent dyspnea. Endoscopic studies showed an adequate supraglottic and glottic space but with the immobility of the residual infraglottic epiglottis. Pulmonology evaluation detected pulmonary involvement due to the progression of the xanthogranulomatous disease. A tracheostomy was performed, improving inspiratory dyspnea. Cladribine treatment was initiated [4-6].
Excessive proliferation of histiocytes results in tumors that can affect various organs. Diseases caused by histiocytes can be classified by the World Health Organization into Langerhans cell histiocytosis, non-Langerhans cell histiocytosis, and malignant histiocytosis. Langerhans cells can be identified with immunohistochemical techniques as positive for CD1a and S100, whereas non-Langerhans cell histiocytosis is negative for these markers.
Juvenile xanthogranulomatosis is a rare benign disease, representing 0.5% of tumors in children, and is the most common form of non-Langerhans cell histiocytosis. It originates from a proliferation of dendritic cells, positive for factor XIIIa, which is presumed to be the precursor of many dendritic disorders in mucocutaneous histiocytosis. It manifests as red, orange, yellow, or brown nodules or papules and is usually self-limiting.
Multiple skin lesions may appear in 10% of patients, and visceral involvement is even rarer.
Adult xanthogranulomatosis is very rare and affects individuals between 20 and 40 years of age.
Skin involvement in the head and neck region is more common, but it can be disseminated and affect the lungs, long bones, retroperitoneum, and other organs. It may rarely be associated with myelodysplastic syndromes, acute lymphoblastic leukemia, and neurofibromatosis.
Laryngeal xanthogranuloma in adults is extremely rare. A review of the English literature found 10 reported cases with laryngeal involvement, seven of which were juvenile and three were adult xanthogranulomatosis. In the juvenile form, the most common symptom was dyspnea, and two of the seven patients required tracheostomy. The most common laryngeal location was the subglottis (6/7), followed by involvement of the aryepiglottic folds (2/7). In the three adult cases, lesions were located on the vocal cords (2/3) and subglottis (1/3).
Surgical intervention is indicated if the lesion causes laryngeal symptoms. In the described case, the transoral epiglottectomy temporarily resolved the inspiratory dyspnea. Subsequently, a tracheostomy was necessary due to the reappearance of inspiratory dyspnea, possibly due to the rigidity and immobility of the residual epiglottis.
When xanthogranulomas are unresectable or surgery is deemed unacceptable due to morbidity, chemotherapy or radiotherapy may be considered, although their benefit for treating xanthogranuloma in adults has not been established. Reports of their use exist for other non-Langerhans cell histiocytosis. Many of these data are extrapolated from treatments for Langerhans cell histiocytosis.
- Li S, Weidenbecher M. Adult onset xanthogranuloma presenting as laryngeal mass. Am J Otolaryngol Head Neck Med Surg. 2015;36(1):84-86. Available from: https://doi.org/10.1016/j.amjoto.2015.10.003
- Weitzman S, Jaffe R. Uncommon histiocytic disorders: the non-Langerhans cell histiocytosis. Pediatr Blood Cancer. 2005;45(3):256-264. Available from: https://doi.org/10.1002/pbc.20246
- Luder CM, Nordmann TM, Ramelyte E, Mühleisen B, Kerl K, Guenova E, et al. Histiocytosis – cutaneous manifestations of hematopoietic neoplasm and non-neoplastic histiocytic proliferations. J Eur Acad Dermatol Venereol. 2018;32(1):926-934. Available from: https://doi.org/10.1111/jdv.14794
- Popa LL, Mihai MM, Orzan LO, Beiu C, Tebeica T, Giurcaneanu C. Adult onset xanthogranuloma – case report and review of literature. Rev Med Rom. 2019;66(4):22-30. Available from: https://rmj.com.ro/articles/2019.4/RMJ_2019_4_Art-22.pdf
- Meyer SN, Vaughn A, Li Y, Studer AC, Rauen KA, Kiuru M. The association between juvenile xanthogranulomas in neurofibromatosis type 1 patient and the development of leukemia: A systematic review. J Eur Acad Dermatol Venereol. 2023;37(12). Available from: https://doi.org/10.1111/jdv.19321
- Velletrani GL, Francavilla B, Rosati V, Padial B, Anemona L, Di Girolamo S. Adult onset xanthogranuloma presenting as a solitary laryngeal localization: case report and review of literature. Arch Clin Cases. 2022;9(4):145-149. Available from: https://doi.org/10.22551%2F2022.37.0904.10221