More Information
Submitted: April 04, 2025 | Approved: April 15, 2025 | Published: April 16, 2025
How to cite this article: Tulachan B, Acharya R. Success Rate and Complications of Endoscopic Deacryocystorhinostomy without Stenting: A Retrospective Study. Heighpubs Otolaryngol Rhinol. 2025; 9(1): 001-004. Available from:
https://dx.doi.org/10.29328/journal.hor.1001030.
DOI: 10.29328/journal.hor.1001030
Copyright license: © 2025 Tulachan B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Endoscopic; Dacryocystorhinostomy; Aesthetic
Abbreviations: EDCR: Endoscopic Dacryocystorhinostomy; NLDO: Nasolacrimal Duct Obstruction; ORL-HNS: Otorhinolaryngology Head and Neck Surgery; UCMS,TH: Universal College of Medical Sciences, Teaching Hospital; DNS; Deviated Nasal Septum; POD: Postoperative Day; CB: Concha Bullosa; NPL: Nasopharyngolaryngoscopy
Success Rate and Complications of Endoscopic Deacryocystorhinostomy without Stenting: A Retrospective Study
Tulachan B1* and Acharya R2
1Associate Professor and Head of Department, Universal College of Medical Sciences, Nepal
2Lecturer, Universal College of Medical Sciences, Nepal
*Address for Correspondence: Dr. Bishow Tulachan, Associate Professor, Department of ENT-Head and Neck Surgery, Universal College of Medical Sciences, Nepal, Email: [email protected]; [email protected]
Endoscopic dacryocystorhinostomy (EDCR) is a well accepted surgical treatment for patients with nasolacrimal duct obstruction (NLDO). Previously, external dacryocystorhino-stomy was considered as the gold standard treatment for NLDO, however, EDCR has gained momentum due to its several advantages. The EDCR has been sounding more aesthetic and as functional compared to the traditional external dacryocystorhinostomy in the surgical treatment of nasolacrimal duct obstruction with comparable outcomes.
Purpose: to determine the success rate and complications of endoscopic dacryocystorhinostomy without stenting.
Materials and methods: it was a retrospective study performed in the department of Otorhinolaryngology and Head and Neck Surgery (ORL-HNS), Universal College of Medical Sciences-Teaching Hospital (UCMS-TH) from June 2019 to September 2024. A total of 19 patients charts were reviewed. All the cases were performed under general anesthesia. All the cases had undergone without silicon stenting and were regularly followed up for a period of 3 months. Post operative stomal patency and complications were noted based on subjective and endoscopic evaluation.
Results: Out of 19 patients, 12 were female and 7 were male with the age range of 12 to 70 years. Transnasal synechiae was seen in 2 female and 1 male patients. Stomal patency was 100% with no recurrence of epiphora in 17 patients (89.4%) during 3 months of follow up. 2 female patients with released synechiae didn’t come for 3 months follow up.
Conclusion: It is a safe and minimally invasive procedure and has a comparable success rate to external DCR with an additional advantage of more aesthetic value.
Endoscopic Dacryocystorhinostomy (DCR) is a well accepted surgical treatment for patients with Nasolacrimal Duct Obstruction (NLDO). Previously, External Dacryocystorhino-stomy (EDCR) was considered as the gold standard treatment for NLDO. Owing the significant advantages and comparable success rate, endoscopic DCR has evolved as an alternative treatment. The advantages of EDCR over external DCR include a lack of external skin scar, preservation of the pump function of the orbicularis oculi muscle, minimal risk of bleeding, early postoperative recovery time and less operating time. The overall success rate of EDCR has been mentioned as 82-98% in the literature [1-9].
The dacryocystorhinostomy restores the patency of the lacrimal drainage system by creating a fistula between lacrimal sac and nasal cavity for the drainage of tears [9,10]. Intranasal DCR was first described by Caldwell in1893. Intranasal technique was not favored meantime due to poor visibility of intranasal anatomy. Post introduction of high resolution fiber-optic endoscopes and rigid endoscopes with different degrees of angulations intranasal technique gained momentum. McDonogh and Meiring introduced endoscopic trans-nasal dacryocystorhinostomy in 1989 [10-16].
Several studies have opted that the granulations, synechiae and even the use of silicon intubation leading to granulation tissue formation postoperatively as factors leading to high failure rates due to obstruction of neo-ostium [17-22].
Our center frequently receives the referred cases of chronic NLDO from the Eye institutes to rule out the nasal abnormalities so that they can perform external DCR without any complications and achieve excellent outcomes. We’ve been performing endoscopic DCR in surgically indicated NLDO patients with endonasal abnormalities and also those wishing for scar free surgery. The objective of this study was to evaluate the success rate and complications of endoscopic DCR without the use of stent.
A retrospective study was done going through the medical records of all EDCR patients in Universal College of Medical Sciences-Teaching Hospital (UCMS-TH) from June 2019 to September 2024. 19 patients files were reviewed. Ethical approval (UCMS/IRC/105/24) was obtained from instituitional review committee of the UCMS. Referred cases from eye institute diagnosed with chronic NLDO planned for external DCR were included. All cases were above 12 years of age. Patients with nasal granulomatous diseases like atrophic rhinitis, neoplastic conditions of sinonasal and nasolacrimal system and the revision cases were excluded.
Age, sex, endonasal pathology, laterality, duration of surgery, endoscopic DCR only or with endonasal pathology correction (septoplasty / Submucosal resection / concha bullosa resection / functional endoscopic sinus surgery), complications (hemorrhage, transnasal synechia, epiphora, periorbital emphysema or edema, peri rhinostomy granuloma or crusting) and outcomes were recorded in the performa. Data were entered in the MS Excel and analyzed. Outcomes were noted in terms of the functional success: subjective improvement of epiphora as reported by the patient at 3 months follow-up ((relief of symtoms) and the anatomical success: endoscopic examination of neo ostium and patent syringing at 3 months follow-up. Failure was defined as absence of symptom relief, closed ostium on endoscopy and not patent on irrigation.
Surgical procedure
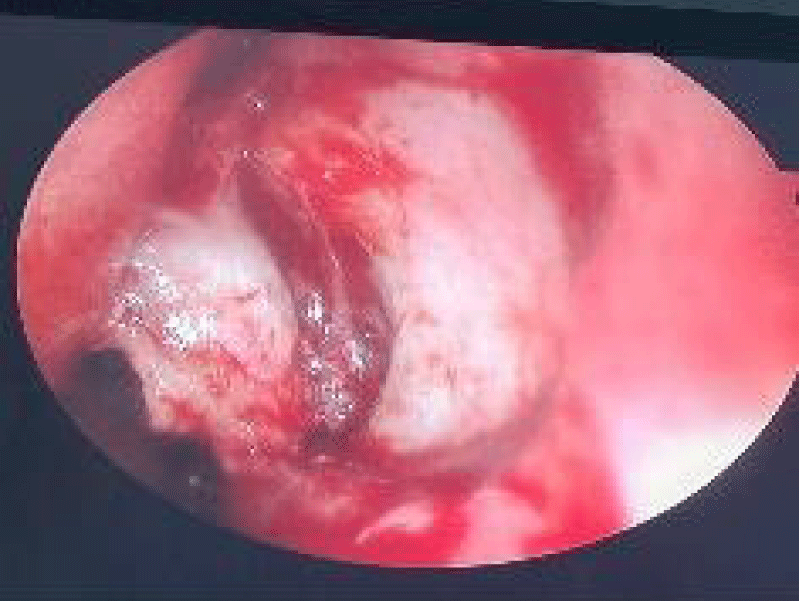
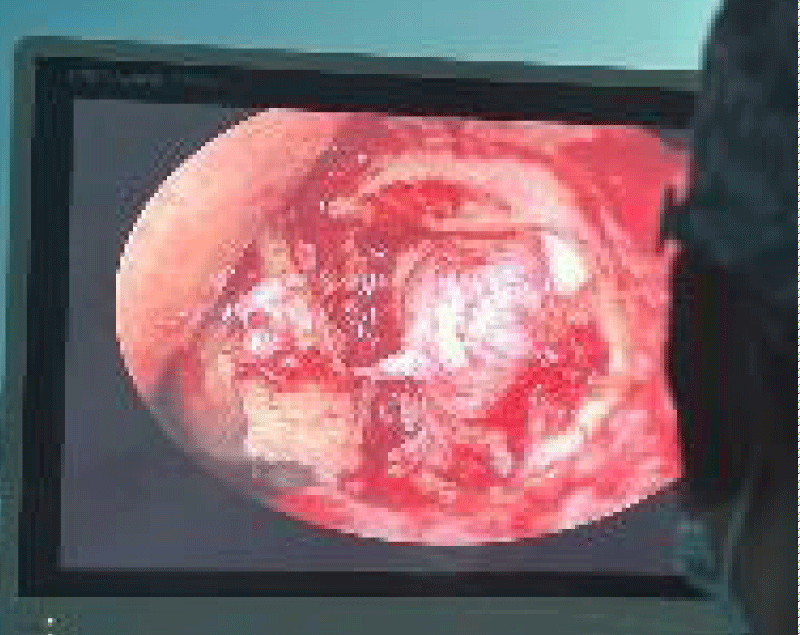
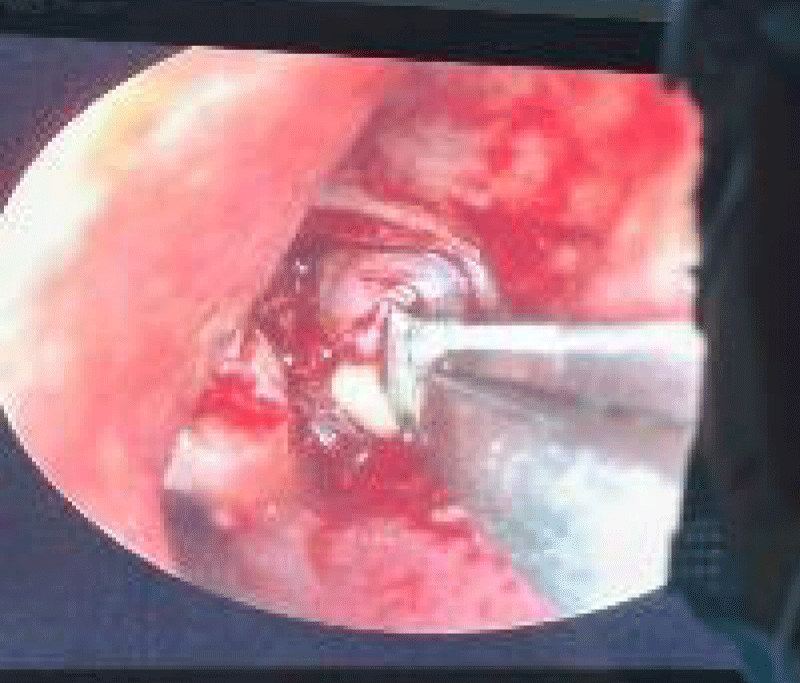
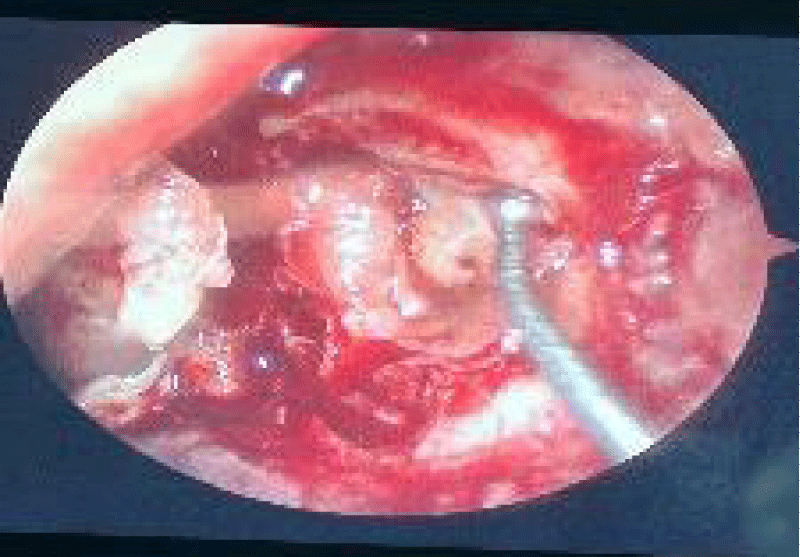
All the cases were done under general anesthesia. Patients with DNS underwent endoscopic septoplasty followed by EDCR. Septal incision was made contralateral to DCR side. Injection 2% Xylocaine with 1:200000 Adrenaline around 10 ml were locally infiltrated into the incision site. After the completion of septoplasty, ribbon gauze impregnated with oxymetazoline nasal drops were kept in the nasal cavity for 5 minutes so as to have better access. Incision was made anterior to the uncinated process. The first horizontal incison was made around 8-9mm above the axilla and proceeding 2cm anteriorly. The second horizontal incision was made on top of the inferior turbinate and the two incisions were joined by the vertical incision by a 15 number scalpel blade. Mucoperiosteal flap was elevated with the help of suction elevator posteriorly upto the uncinate process (Figure 1). Lacrimal bone was palpated and removed with the help of Kerrison’s bone punch forceps and coarse diamond burr and the entire lacrimal duct was exposed superiorly upto the common cannaliculus and inferiorly to nasolacrimal duct (Figure 2). A 12 number scalpel blade and a ball probe was used to open the nasolacrimal duct (Figure 3). In all the patients there was presence of mucopurulent discharge once the sac was opened and cleansing was done with the betadine mixed saline solution. Anterior and posterior flaps were created and the duct was completely marsupialized (Figure 4). A few pieces of gelfoam were kept for the flaps support. Mucoperiosteal flap was then cut into two halves in the midline and the raw bone were covered keeping the stoma open. Loose anterior nasal packing was done bilaterally (Figure 5). Pack was removed after 48 hours and discharged on the next day. Injection Ceftriaxone 1gm twice daily, tablet Flexon (paracetamol+Ibuprofen) thrice daily and tablet Fexofenadine 120mg once daily were given to the patient. Post pack removal oxymetazoline nasal drops, saline nasal drops, ciprofloxacin ointment were applied in the nasal cavity. Saline drops, Ciprofloaxin ointment and Fexofenadine tablet were continued for 1 month. Patients were followed up at 7th post operative day (POD), 14th POD and after 3 months (Figure 6). At each visit patients were asked for symptomatic relief (watering from the eyes) and endonasal assessment of the stoma and the syringing of eye and the findings were noted.
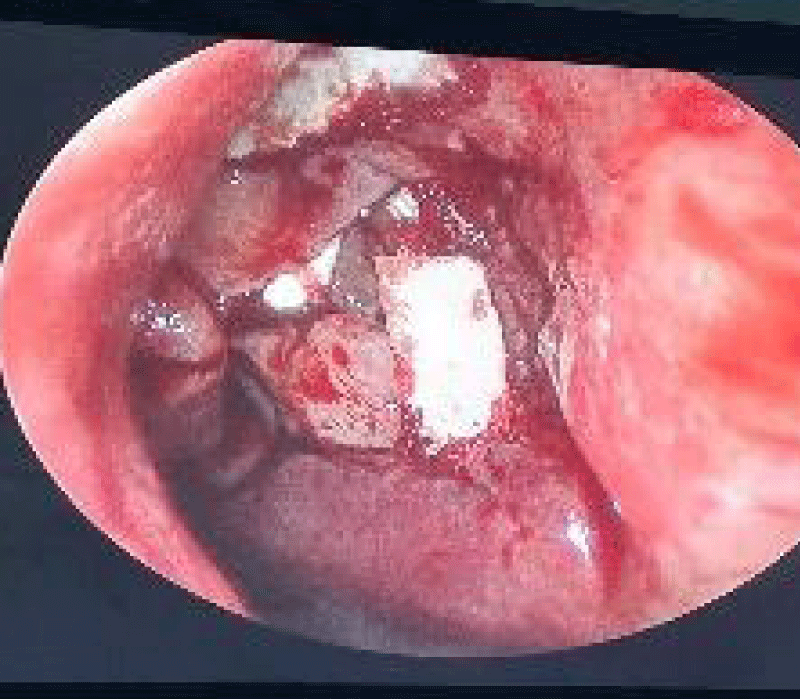
Figure 1: Bony nasolacrimal system after flap elevation.
Figure 2: Nasolacrimal duct.
Figure 3: Opening of NLD with scalpel blade 12, creation of anterior and posterior flaps and marsupialization completed with gelfoam support on flaps and repositioning of initial flaps to cover the raw bones.
Figure 4: Opening of NLD with scalpel blade 12, creation of anterior and posterior flaps and marsupialization completed with gelfoam support on flaps and repositioning of initial flaps to cover the raw bones.
Figure 5: Opening of NLD with scalpel blade 12, creation of anterior and posterior flaps and marsupialization completed with gelfoam support on flaps and repositioning of initial flaps to cover the raw bones.
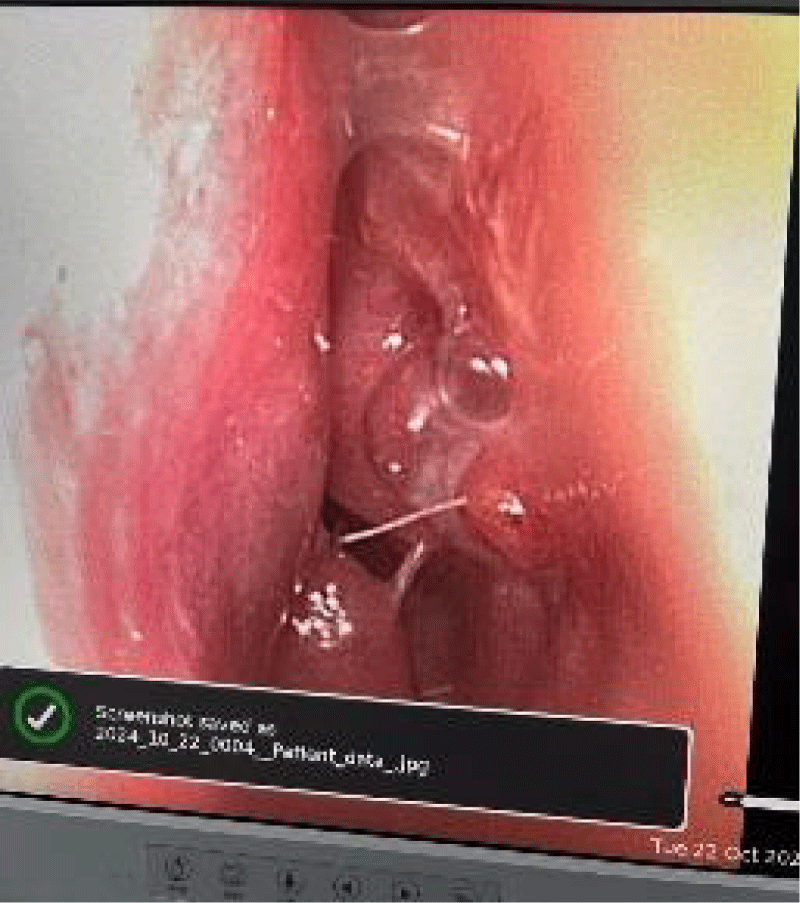
Figure 6: Patent neo ostium at 3 months follow up.
Out of 19 patients, 12 were female and 7 were male with the age range of 12 to 70 years. Intranasal synechiae was seen between the inferior turbinate and the septum in 2 female and 1 male patients and were released under LA in 14th POD. Stomal patency was 100% with no recurrence of epiphora in 17 patients during 3 months of follow up. 2 female patients with synechiae lost to follow up. All the patients had nasal pathology (Table 1).
| Table 1: Preoperative endonasal pathology. | ||
| Nasal pathology | No. of patients (n = 19) | Percentage |
| Deviated nasal septum (DNS) | 15 | 78.94% |
| DNS with spur | 4 | 21.05% |
| Chronic rhinosinusitis (CRS) | 0 | 0 |
| Concha bullosa (CB) | 0 | 0 |
| Nasal polyps | 0 | 0 |
During endonasal assessment, 15 patients had high DNS (78.94%)) and DNS with spur in 4 patients (21.05%)). Enodoscopic septoplasty and DCR were done at same sitting in all patients. DCR was performed in 11 left and 8 right eyes. The duration of surgery was approximately 1 hour and 45 minutes. Intranasal synechiae was seen in 2 female and 1 male patients in DNS with spur group. They were 70 years male and 37 and 23 years female. Synechiae was successfully released under local anesthesia in out-patient setting. However 2 female patients post synechiae release didn’t show up in 3 months follow up. Subjectively patients had complete relief (no watering of eyes) at 3 months follow up in 17 patients (89.4%). At each follow up, there was a free flow during syringing of the operated eyes. Fiberoptic nasopharyngolaryngoscopy (NPL) was performed on each visit. There was no granuloma or granulation tissue around the stomal site at 3 months follow up.
The aim of this study was to find out the success rate and complications of EDCR in our institute UCMS, TH. DCR is a commonly done procedure to treat nasolacrimal duct obstruction. It’s being done either externally or intranasally. Endoscopic DCR has fascinated a lot of surgeons and the patients due to its certain positive aspects and also the success rate being almost similar to external approach [1-9]. Till date there’s no publication regarding the standard criterion to evaluate the success rates of lacrimal surgery. Different studies have used different criteria of success and varying patient selection. The Royal collage of ophthalmologist published guideline for clinical governance suggesting that freedom from epiphora 3 months after surgery is the marker for satisfactory procedure [8].
Rice had a 100% success rate of EDCR (n = 4). Whittet reported (n = 40) 83% success rate of EDCR. Weidenbocher from Germany had an 86% success rate. Camara had reported the success rate of EDCR ranging from 70% to 95 %. Sprekelson had reported a large series of patients and had a 96% success rate. Singhal SK, et al. had reported 89.7% success rate without intubation [8]. Shrestha, et al. study had reported the success rate of 84% of EDCR without intubation [17]. Ramakrishnan, et al. had 100% success rate on anatomic patency and 93% on complete resolution of epiphora (27 EDCR in 20 patients from 2003 to 2006).11Several studies had encountered complications like eyelid edema, granuloma and fibrosis around neo-ostium, epiphora recurrence and intranasal synechia post surgery and has been considered to be the reasons for failure of EDCR. Our success rate of EDCR (89.4%) and the complications faced was similar to the rates (81% - 87%) reported without intubation [10,11,13,17,22]. So, there are varied outcomes on success rates and the complications of EDCR.
The limitations of the study is the small sample size and its retrospective nature.
EDCR without stent is an effective, safe and minimally invasive primary procedure for the treatment of nasolacrimal duct obstruction with comparable outcomes to external DCR and more of aesthetic value.
The proper selection of the patient, the meticulous surgery and the early tackling of the postoperative complications would yield a higher success and more satisfaction to both the operating surgeons and the patients compared to the external approach.
- Sung JY, Lee YH, Kim KN, Kang TS, Lee SB. Surgical outcomes of endoscopic dacryocystorhinostomy: analysis of age effect. Sci Rep. 2019;9:19861. Available from: https://doi.org/10.1038/s41598-019-56491-y
- Neil F, Jones NS. Dacryocystorhinostomy. In: Gleeson M, editor. Scott-Brown’s Otorhinolaryngology, Head and Neck Surgery. London: Edward Arnold Ltd; 2008;1689–98.
- Mak ST, Io IY, Wong AC. Prognostic factors for outcome of endoscopic dacryocystorhinostomy in patients with primary acquired nasolacrimal duct obstruction. Graefes Arch Clin Exp Ophthalmol. 2013 May;251(5):1361–7. Available from: https://doi.org/10.1007/s00417-012-2228-9
- Leong SC, Macewen CJ, White PS. A systematic review of outcomes after dacryocystorhinostomy in adults. Am J Rhinol Allergy. 2010 Jan-Feb;24(1):81–90. Available from: https://doi.org/10.2500/ajra.2010.24.3393
- Coumou AD, Genders SW, Smid TM, Saeed P. Endoscopic dacryocystorhinostomy: long-term experience and outcomes. Acta Ophthalmol. 2017 Feb;95(1):74–8. Available from: https://doi.org/10.1111/aos.13217
- Ali MJ, Psaltis AJ, Bassiouni A, Wormald PJ. Long-term outcomes in primary powered endoscopic dacryocystorhinostomy. Br J Ophthalmol. 2014 Dec;98(12):1678–80. Available from: https://doi.org/10.1136/bjophthalmol-2014-305510
- Yung MW, Hardman-Lea S. Analysis of the results of surgical endoscopic dacryocystorhinostomy: effect of the level of obstruction. Br J Ophthalmol. 2002 Jul;86(7):792–4. Available from: https://doi.org/10.1136/bjo.86.7.792
- Ben Simon GJ, Joseph J, Lee S, Schwarcz RM, McCann JD, Goldberg RA. External versus endoscopic dacryocystorhinostomy for acquired nasolacrimal duct obstruction in a tertiary referral center. Ophthalmology. 2005 Aug;112(8):1463–8. Available from: https://doi.org/10.1016/j.ophtha.2005.03.015
- Karpishchenko SA, Vereshchagina OE, Baranskaya S, Karpov AA. Rhinological Aspects of Endonasal Endoscopic Dacryocystorhinostomy. Glob J Otolaryngol. 2018;14(4):1–4. Available from: http://dx.doi.org/10.19080/GJO.2018.14.555895
- Ayoob M, Mahida K, Qurat-ul-ain, Dawood Z. Outcome and complications of endoscopic dacryocystorhinostomy without stenting. Pak J Med Sci. 2013 Sep-Oct;29(5):1236–9. Available from: https://doi.org/10.12669/pjms.295.3393
- Pradhan B. Outcome of endoscopic DCR at TUTH. Nepal J ENT Head Neck Surg. 2011;2(1):20–1. Available from: https://doi.org/10.3126/njenthns.v2i1.6780
- Tan NC, Rajapaksa SP, Gaynor J, Nair SB. Mechanical endonasal dacryocystorhinostomy—a reproducible technique. Rhinology. 2009;47(3):310–5. Available from: https://doi.org/10.4193/Rhin08.150
- Mortimore S, Banhegyi GY, Lancaster JL, Karkanevatos A. Endoscopic dacryocystorhinostomy without silicone stenting. J R Coll Surg Edinb. 1999;44(6):371–3. Available from: https://pubmed.ncbi.nlm.nih.gov/10612959/
- Aslam S, Awan AH, Tayyab M. Endoscopic dacryocystorhinostomy: a Pakistani experience. Pak J Ophthalmol. 2010;26(1):2–6. Available from: https://pjo.org.pk/index.php/pjo/article/view/595
- Yuen KSC, Lam LYM, Tse MWY. Modified endoscopic dacryocystorhinostomy with posterior lacrimal flap for nasolacrimal duct obstruction. Hong Kong Med J. 2004;10(6):394–400. Available from: https://pubmed.ncbi.nlm.nih.gov/15591598/
- Kakar V, Chugh JP, Sachdeva S, Sharma N, Ramesh. Endoscopic dacryocystorhinostomy with and without silicone stent: a comparative study. Internet J Otorhinolaryngol. 2009;9(1).
- Shrestha S, Kafle PK, Pokhrel S, Maharjan M, Toran KC. Success rate of endoscopic dacryocystorhinostomy at KMC. Kathmandu Univ Med J. 2010;8(30):195–8. Available from: https://doi.org/10.3126/kumj.v8i2.3557
- Hamal D, Kafle PA, Lamichhane B, Anwar A, Singh SK. Endoscopic endonasal dacryocystorhinostomy under local anesthesia or assisted local anesthesia. Nepal J Ophthalmol. 2022;14(1):10–8. Available from: https://doi.org/10.3126/nepjoph.v14i1.21971
- Abdu L, Bawahab N, Mohammed Hussain RW, Qary H, Saeedi A, Alhibshi N. Prevalence and treatment outcome of nasolacrimal duct obstruction in Saudi children with Down syndrome. Cureus. 2020;12(1):e6672. Available from: https://doi.org/10.7759/cureus.6672
- Hehar SS, Jones NS, Sadiq A, Downes RN. Endoscopic holmium: YAG laser dacryocystorhinostomy is safe and effective as a day care procedure. J Laryngol Otol. 1997;111(11):1056–9. Available from: https://doi.org/10.1017/s0022215100139325
- Unlu HH, Toprak B, Aslan A, Guler C. Comparison of surgical outcomes in primary endoscopic dacryocystorhinostomy without silicone intubation. Ann Otol Rhinol Laryngol. 2002;111(8):704–9. Available from: https://doi.org/10.1177/000348940211100809
- Yang JW, Oh HN. Success rate and complications of endonasal dacryocystorhinostomy with unciformectomy. Graefes Arch Clin Exp Ophthalmol. 2012;250(10):1509–13. Available from: https://doi.org/10.1007/s00417-012-1992-x